Lilly's bamlanivimab and etesevimab together reduced hospitalizations and death in Phase 3 trial for early COVID-19
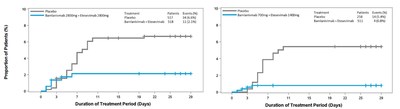
This new Phase 3 cohort of BLAZE-1 included 769 high-risk patients, aged 12 and older with mild to moderate COVID-19 (therapy: n=511; placebo: n=258). There were four events in patients taking bamlanivimab with etesevimab and 15 events in patients taking placebo, representing an 87 percent risk reduction (p<0.0001). Bamlanivimab and etesevimab together also demonstrated statistically significant improvements on key secondary endpoints. These results are consistent with those seen in other data sets from BLAZE-1: in the previous Phase 3 cohort, bamlanivimab 2800 mg with etesevimab 2800 mg reduced the risk of hospitalizations and deaths by 70 percent and in the Phase 2 cohort, bamlanivimab alone reduced the risk of hospitalizations and ER visits by approximately 70 percent. The viral load reductions were also consistent with what was observed in the previous Phase 3 cohort of the study.
In this new Phase 3 cohort, there were four deaths total, all of which were deemed related to COVID-19 and all of which occurred in patients taking placebo; no deaths occurred in patients receiving treatment with bamlanivimab and etesevimab together. Across the two Phase 3 cohorts of the study that have been analyzed to date, there have been no deaths in patients receiving treatment with bamlanivimab and etesevimab together, and 14 deaths in patients receiving placebo, 13 of which were deemed COVID-19 related. In this data set, the safety profile of bamlanivimab and etesevimab together was consistent with observations from other Phase 1, Phase 2 and Phase 3 trials evaluating these antibodies.
"These positive results reinforce our previous findings and support the authorized dose of bamlanivimab 700 mg with etesevimab 1400 mg. These compelling data – in addition to the recent EUA from FDA, the CHMP decision from EMA and the recommendation for the therapy in the
For more information about the use of bamlanivimab alone or bamlanivimab and etesevimab together for the treatment of mild to moderate COVID-19 in high-risk patients under the
For media resources, including product images and fact sheets, please click here.
Important Information about bamlanivimab alone and bamlanivimab and etesevimab together
Bamlanivimab and etesevimab together and bamlanivimab alone have not been approved by the FDA for any use. It is not known if bamlanivimab and etesevimab together or bamlanivimab alone are safe and effective for the treatment of COVID-19.
Bamlanivimab and etesevimab together and bamlanivimab alone are authorized under Emergency Use Authorization only for the duration of the declaration that circumstances exist justifying the authorization of the emergency use under Section 564(b)(1) of the Act, 21 U.S.C § 360bbb-3(b)(1), unless the authorization is terminated or revoked sooner.
Healthcare providers should review the Fact Sheet for information on the authorized use of bamlanivimab and etesevimab together and bamlanivimab alone and mandatory requirements of the EUA. Please see the FDA Letter of Authorization, Fact Sheet for Healthcare Providers, and Fact Sheet for Patients, Parents and Caregivers (English) (Spanish) for bamlanivimab and etesevimab together. Please see the FDA Letter of Authorization, Fact Sheet for Healthcare Providers, and Fact Sheet for Patients, Parents and Caregivers (English) (Spanish) for bamlanivimab alone.
Authorized Use and Important Safety Information
Bamlanivimab and etesevimab together and bamlanivimab alone are authorized for use under EUA for treatment of mild to moderate COVID-19 in adults and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progressing to severe COVID-19 and/or hospitalization.
Limitations of Authorized Use
- Bamlanivimab and etesevimab together and bamlanivimab alone are not authorized for use in patients:
- who are hospitalized due to COVID-19, OR
- who require oxygen therapy due to COVID-19, OR
- who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy due to underlying non-COVID-19 related comorbidity.
- Treatment with bamlanivimab and etesevimab together has not been studied in patients hospitalized due to COVID-19. Benefit of treatment with bamlanivimab alone has not been observed in patients hospitalized due to COVID-19. Monoclonal antibodies, such as bamlanivimab and etesevimab, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation.
Important Safety Information
There are limited clinical data available for bamlanivimab and etesevimab together and bamlanivimab alone. Serious and unexpected adverse events may occur that have not been previously reported with bamlanivimab and etesevimab together and bamlanivimab alone.
Hypersensitivity Including Anaphylaxis and Infusion-Related Reactions
Serious hypersensitivity reactions, including anaphylaxis, have been observed with administration of bamlanivimab and etesevimab together and bamlanivimab alone. If signs and symptoms of a clinically significant hypersensitivity reaction or anaphylaxis occur, immediately discontinue administration and initiate appropriate medications and/or supportive care.
Infusion-related reactions have been observed with administration of bamlanivimab and etesevimab together and bamlanivimab alone. These reactions may be severe or life threatening. Signs and symptoms of infusion-related reactions may include:
- fever, difficulty breathing, reduced oxygen saturation, chills, fatigue, arrhythmia (e.g. atrial fibrillation, sinus tachycardia, bradycardia), chest pain or discomfort, weakness, altered mental status, nausea, headache, bronchospasm, hypotension, hypertension, angioedema, throat irritation, rash including urticaria, pruritus, myalgia, dizziness, and diaphoresis.
If an infusion-related reaction occurs, consider slowing or stopping the infusion and administer appropriate medications and/or supportive care.
Clinical worsening of COVID-19 after administration of bamlanivimab has been reported and may include signs or symptoms of fever, hypoxia or increased respiratory difficulty, arrhythmia (e.g., atrial fibrillation, sinus tachycardia, bradycardia), fatigue, and altered mental status. Some of these events required hospitalization. It is not known if these events were related to bamlanivimab use or were due to progression of COVID-19.
Limitations of Benefit and Potential Risk in Patients with Severe COVID-19
Treatment with bamlanivimab and etesevimab together has not been studied in patients hospitalized due to COVID-19. Benefit of treatment with bamlanivimab alone has not been observed in patient hospitalized due to COVID-19. Monoclonal antibodies, such as bamlanivimab and etesevimab, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation. See Limitations of Authorized Use.
Adverse Events
Bamlanivimab and etesevimab together
Based on Phase 2 data from BLAZE-1, nausea was the most commonly reported adverse event, reported by 4% of subjects in both bamlanivimab and etesevimab together and placebo groups. Pruritus and pyrexia were more frequently reported from subjects treated with both bamlanivimab and etesevimab (2% and 1%) compared to placebo (1% and 0%, respectively).
Based on Phase 3 data from BLAZE-1, the most common adverse events were nausea, dizziness, and rash. These events each occurred in 1% of subjects treated with bamlanivimab and etesevimab together and in 1% of placebo subjects.
Bamlanivimab alone
Adverse events reported in at least 1% of BLAZE-1 clinical trial participants on bamlanivimab 700 mg alone or placebo were nausea (3% vs 4%), diarrhea (1% vs 5%), dizziness (3% vs 2%), headache (3% vs 2%), pruritus (2% vs 1%) and vomiting (1% vs 3%).
Use in Specific Populations
Pregnancy
There are insufficient data on the use of bamlanivimab and etesevimab together and bamlanivimab alone during pregnancy. Bamlanivimab and etesevimab together and bamlanivimab alone should only be used during pregnancy if the potential benefit outweighs the potential risk for the mother and the fetus.
Breastfeeding
There are no available data on the presence of bamlanivimab or etesevimab in human or animal milk, the effects on the breastfed infant, or the effects on milk production. Breastfeeding individuals with COVID-19 should follow practices according to clinical guidelines to avoid exposing the infant to COVID-19.
About bamlanivimab
Bamlanivimab is a recombinant, neutralizing human IgG1 monoclonal antibody (mAb) directed against the spike protein of SARS-CoV-2. It is designed to block viral attachment and entry into human cells, thus neutralizing the virus, potentially treating COVID-19. Bamlanivimab emerged from the collaboration between
About etesevimab
Etesevimab (LY-CoV016, also known as JS016) is a recombinant fully human monoclonal neutralizing antibody, which specifically binds to the SARS-CoV-2 surface spike protein receptor binding domain with high affinity and can block the binding of the virus to the ACE2 host cell surface receptor. Point mutations were introduced into the native human IgG1 antibody to mitigate effector function.
About BLAZE-1
BLAZE-1 (NCT04427501) is a randomized, double-blind, placebo-controlled Phase 2/3 study designed to assess the efficacy and safety of bamlanivimab alone or bamlanivimab and etesevimab together for the treatment of symptomatic COVID-19 in the outpatient setting. To be eligible, patients were required to have mild or moderate symptoms of COVID-19 as well as a positive SARS-CoV-2 test based on a sample collected no more than three days prior to drug infusion.
In the Phase 2 portion of BLAZE-1, cohorts of mild to moderate recently diagnosed COVID-19 patients, were randomized to one of three doses of bamlanivimab (700 mg, 2800 mg, and 7000 mg), bamlanivimab 2800 mg plus etesevimab 2800 mg, or placebo. Results from the Phase 2 cohorts of BLAZE-1 were published in the
In the Phase 3 portion of BLAZE-1, the combination therapy arms enrolled mild to moderate, recently diagnosed COVID-19 patients who are at high risk for progressing to severe COVID-19 and/or hospitalization, studying bamlanivimab 2800 mg plus etesevimab 2800 mg versus placebo, and bamlanivimab 700 mg plus etesevimab 1400 mg versus placebo. The primary outcome measure for the Phase 3 portion of the BLAZE-1 trial was the percentage of participants who experience COVID-related hospitalizations or death from any cause by day 29. The key secondary endpoints were change from baseline to day 7 in SARS-CoV-2 viral load, persistently high SARS-CoV-2 viral load on day 7, time to sustained symptom resolution, and COVID-related hospitalization, ER visit or death from any cause from baseline by day 29. Additional endpoints include change from baseline in viral load at other time points, symptom improvement, symptom resolution, as well as safety.
The study is ongoing with additional treatment arms.
About
About Eli
This press release contains forward-looking statements (as that term is defined in the Private Securities Litigation Reform Act of 1995) about bamlanivimab (LY-CoV555) alone or bamlanivimab and etesevimab (LY-CoV016) together as potential treatments for patients with COVID-19, as well as its supply and distribution, and reflects
|
Refer to: |
|
|
|
|
|
|
![]() View original content to download multimedia:http://www.prnewswire.com/news-releases/lillys-bamlanivimab-and-etesevimab-together-reduced-hospitalizations-and-death-in-phase-3-trial-for-early-covid-19-301243984.html
View original content to download multimedia:http://www.prnewswire.com/news-releases/lillys-bamlanivimab-and-etesevimab-together-reduced-hospitalizations-and-death-in-phase-3-trial-for-early-covid-19-301243984.html
SOURCE